Imagine sitting in a hospital waiting room. Not for a routine check-up, but waiting for a call that might never come – the call saying a matching organ is available. This isn’t a hypothetical for millions worldwide; it’s a harsh reality. Every single day, lives are lost because the supply of donor organs simply cannot meet the overwhelming demand. It’s a healthcare crisis that touches families across the globe, leaving doctors and patients alike searching desperately for solutions. This isn’t just a medical problem; it’s a profound human challenge.
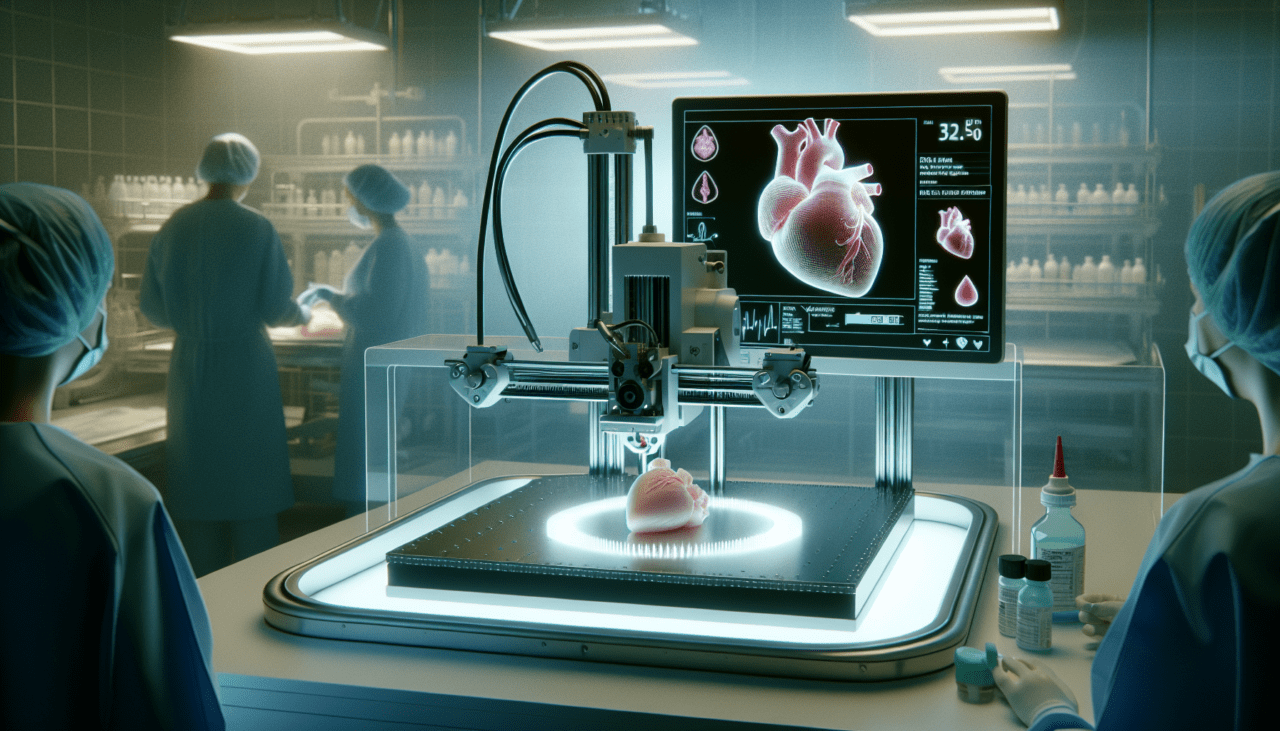
But what if the solution wasn’t dependent on finding a perfect human match? What if we could, essentially, build the organs people need? That’s the incredible promise held within the field of regenerative medicine, specifically in the realm of 3D bioprinting. This cutting-edge technology is moving from science fiction labs into tangible possibilities, offering a beacon of hope for a future where organ scarcity is a problem of the past. The potential implications for healthcare, business, and society are simply staggering.
The Pressing Problem: The Global Organ Shortage Crisis
Let’s be frank: the current system for organ transplantation, while miraculous in its own right, is fundamentally limited by the availability of suitable donors. We rely on the generosity of individuals and their families during times of tragedy, and while that generosity saves countless lives, it can never fully close the gap between the number of organs needed and the number available. This creates a backlog, a waiting list that grows longer each year, filled with names of people whose lives are on hold, or worse, slowly slipping away.
The sheer scale of this shortage is difficult to grasp. In the United States alone, tens of thousands of people are on the national transplant waiting list at any given time. While some will receive the life-saving call, many others will not survive the wait. This isn’t just a statistic; it represents parents, children, friends, and colleagues whose potential and presence are lost to this critical deficit. Addressing this requires looking beyond traditional methods to innovative approaches that can scale and personalize organ creation.
The Current Landscape of Organ Transplants
Today’s transplant system is a complex logistical and medical marvel. It involves donor registration, organ retrieval, matching recipients based on blood type, tissue type, and medical urgency, and rapid transportation and surgery. It’s a race against time from the moment an organ becomes available until it’s successfully transplanted. Success rates are impressive for many organs, but challenges remain, including the need for lifelong immunosuppressant drugs to prevent rejection – drugs that come with their own set of side effects and health risks.
Furthermore, the quality and viability of donor organs can vary, and not every donated organ is suitable for transplantation. There are also significant logistical hurdles in transporting organs across distances while maintaining their viability. This intricate dance, while saving lives daily, highlights the constraints of relying on a finite and unpredictable supply chain. It underscores the urgent need for alternative sources of transplantable organs that are readily available, customizable, and potentially less prone to rejection.
The Scale of the Need
The number of people needing transplants isn’t static; it’s influenced by rising rates of chronic diseases like diabetes, heart disease, and liver failure. Kidneys are the most needed organs, followed by livers, hearts, and lungs. Each organ type presents its own unique challenges for donation and transplantation. For example, heart and lung donors must meet very specific criteria, making them particularly scarce.
The waiting list is not just a static tally; it represents a dynamic and often heartbreaking situation where individuals deteriorate while hoping for a match. For businesses involved in healthcare, pharmaceuticals, or medical technology, understanding the depth of this need is crucial. It highlights a massive unmet medical need that innovative solutions like 3D bioprinting could potentially address, opening up significant market opportunities while simultaneously tackling a major humanitarian issue.
How 3D Bioprinting Works for Organs
Okay, so how does 3D printing go from making plastic toys to potentially printing functional organs? It’s a far more complex process than simply layering plastic. We’re talking about bioprinting, which uses biological materials – living cells, growth factors, and biomaterials – often referred to collectively as “bioinks.” These bioinks are carefully deposited layer by layer using specialized 3D printers to create three-dimensional structures that mimic the complexity of biological tissues and organs.
Think of it like building with incredibly tiny, living bricks. Scientists start with patient-specific cells, perhaps derived from a biopsy. These cells are mixed with a bioink, which provides structural support and a friendly environment for the cells to live and grow. The printer then follows a digital blueprint, often created from medical scans of a patient’s own anatomy, to deposit the bioink in precise patterns. The goal is to replicate not just the shape of an organ, but its intricate internal architecture, including blood vessels and other necessary structures.
The Technology Behind Bioprinting
At its core, bioprinting uses techniques similar to traditional 3D printing (like extrusion, inkjet, or laser-assisted printing) but adapted for biological materials. The printer head deposits droplets or streams of bioink onto a build platform, layer by layer, based on a sophisticated computer model. The key is maintaining cell viability and functionality throughout the printing process and afterward. This requires extremely gentle handling and precise environmental control.
Different bioprinting methods are used depending on the desired resolution and the type of tissue being printed. For instance:
- Extrusion-based bioprinting: Pushing bioink through a nozzle, good for creating larger structures but with lower resolution.
- Inkjet-based bioprinting: Dropping bioink like an inkjet printer, offering high speed but can damage cells.
- Laser-assisted bioprinting: Using a laser to deposit bioink from a ribbon, offering high resolution but can be slower.
Researchers are constantly refining these techniques and developing new bioinks that provide better support, mimic the natural cellular environment more closely, and can be easily integrated with the body’s own tissues once implanted. The material science and engineering aspects of bioprinting are just as critical as the biological ones.
Challenges in Creating Complex Organs
While printing simple tissues like skin or cartilage has seen significant progress, creating complex, fully functional organs like hearts or kidneys is incredibly challenging. The main hurdle is vascularization – building a network of blood vessels within the printed tissue. Just like a city needs roads for delivery, a living organ needs blood vessels to supply nutrients and oxygen to its cells and remove waste products. Without this, the cells deep within a printed structure will quickly die.
Another major challenge is achieving the correct cellular complexity and architecture. Organs aren’t just blocks of one cell type; they have multiple cell types arranged in specific ways, performing coordinated functions. Replicating this intricate organization and ensuring the cells mature and communicate correctly after printing is a massive task. Scientists are working on various strategies, including printing sacrificial materials that can be washed away to leave channels for blood vessels, and using multiple printer heads with different cell types and bioinks. The complexity is immense, but the potential payoff fuels relentless research.
The Promise and Path Ahead for 3D-Printed Organs
Despite the hurdles, the potential benefits of successfully printing functional organs are revolutionary. Imagine a future where a patient needing a kidney transplant doesn’t have to wait years on a list, but can have an organ printed, potentially using their own cells, within weeks or months. This would dramatically reduce waiting times and eliminate the critical issue of organ shortage. The impact on healthcare systems and patient outcomes would be transformative.
Beyond just availability, using a patient’s own cells could significantly reduce or even eliminate the need for powerful immunosuppressant drugs, lowering the risk of rejection and improving long-term health outcomes. This would be a huge leap forward in patient care. The ability to personalize organs – printing them to fit a patient’s exact anatomy – could also improve surgical outcomes and organ function. The Future of Organ Transplants: 3D-Printed Organs isn’t just about supply; it’s about better, safer, and more personalized transplants. Furthermore, printed tissues could be used for drug testing, accelerating pharmaceutical research and reducing the need for animal testing.
Potential Benefits and Applications
The applications extend beyond whole organ replacement. 3D bioprinting is already showing promise in creating simpler tissues for repair or regeneration:
- Skin grafts: For burn victims or reconstructive surgery.
- Cartilage implants: For joint repair.
- Bone scaffolds: To aid bone regeneration after injury.
- Liver tissues: For drug toxicity testing and potentially as temporary support for patients with liver failure.
The ability to create complex tissue models also provides invaluable tools for disease research, allowing scientists to study how diseases progress and how potential therapies work in a more realistic environment than traditional cell cultures. For businesses in the biotech and medical device sectors, this represents a fertile ground for innovation, investment, and market development. The tools, materials, and processes required for bioprinting are themselves significant areas of growth.
Overcoming Obstacles and Regulatory Hurdles
Realizing the full potential of 3D-printed organs requires overcoming substantial obstacles. The scientific and engineering challenges mentioned earlier – vascularization, cellular complexity, maturation – are still areas of active research. Scaling up production from lab-scale prototypes to clinically viable, mass-producible organs is another major hurdle. Consistency, quality control, and ensuring the long-term functionality and safety of printed organs are paramount.
Equally significant are the regulatory pathways. Agencies like the FDA in the US are developing frameworks to evaluate these entirely new types of medical products. Demonstrating safety and efficacy through rigorous preclinical testing and clinical trials will be a lengthy and expensive process. Ethical considerations also need careful navigation, such as who gets access to these technologies and ensuring equitable distribution. For investors and businesses, understanding this regulatory landscape and the long development timelines is crucial for strategic planning in The Future of Organ Transplants: 3D-Printed Organs.
The journey from a 3D printer layering bioink to a fully functional, transplantable organ that lasts for years inside a human body is still long and complex. There will be setbacks, unexpected challenges, and the need for massive investment in research and infrastructure. However, the progress made in the last decade is astonishing, and the pace of innovation is accelerating. We are truly on the cusp of a new era in medicine, one where the limitations imposed by organ scarcity might finally be lifted. The potential to save and improve millions of lives makes this one of the most exciting and important frontiers in healthcare technology today. Businesses looking towards the future of medical innovation should absolutely have 3D bioprinting on their radar.